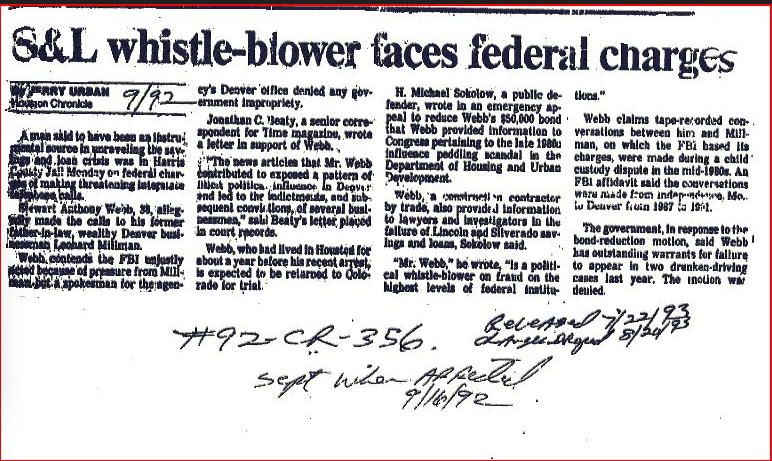
Letter to FBI Director James Comey who coverED up for
FBI James Comey covered up Whistleblower Bret Landrith’s Evidence
Please Copy and Past the Link below into your Browser to View the Evidence:
http://www.stewwebb.com/1-Landrith-Ltr-to-Comey-Attachments-Vol-I.pdf
Dead fired attorneys Medicare fraud probe linked to White House Whistleblower Bret Landrith
Dead fired attorneys Medicare fraud probe linked to White House
FBI James Comey Crossfire Hurricane was involved in 2000 Election Stolen from President Trump
FBI James Comey Crossfire Hurricane was involved in 2000 Election Stolen from President Trump
When Dad Was VP, Jeb Bush Lobbied The Administration For A Medicare Fraudster
https://madisondems.org/2015/02/20/when-dad-was-vp-jeb-bush-lobbied-the-administration-for-a-medicare-fraudster/
by | Feb 20, 2015 | 2016 General Election, Affordable Care Act/Obamacare, News
by Ryan Grim
 WASHINGTON — Jeb Bush personally lobbied the secretary of health and human services, while his father was vice president, on behalf of a Miami figure who would later flee the country accused of one of the greatest Medicare frauds in the program’s history.
WASHINGTON — Jeb Bush personally lobbied the secretary of health and human services, while his father was vice president, on behalf of a Miami figure who would later flee the country accused of one of the greatest Medicare frauds in the program’s history.
Bush pressed then-HHS Secretary Margaret Heckler to give the man’s HMO a waiver so that it could accept larger sums of Medicare money than it otherwise would have been allowed, Heckler told The Huffington Post.
Miguel Recarey Jr., head of the health maintenance organization International Medical Centers (IMC) who often boasted of connections to the Miami Cuban mafia, paid Bush $75,000 in the mid-1980s. Bush has acknowledged receiving the payment but said it was tendered for real estate consultation. But the deal he consulted on was never closed.
The New York Times recently reported that the younger Bush made frequent use of his connection to his father both as vice president and president. “Even within a family long steeped in politics, Mr. Bush stood out to White House aides for the frequency of his communications and the intensity of the opinions,” the paper reported.
Jeb Bush, now a top GOP contender for president in 2016, has addressed the latest criticism by saying that he is his “own man.”
The IMC affair involved hundreds of millions of public dollars. In 1992, as his father, President George H.W. Bush, ran for re-election, Jeb Bush denied having reached out to Heckler on Recarey’s behalf. He said that he had only spoken to a lower-level HHS official to ask that Recarey be given a “fair hearing” with regard to his application to renew a waiver that allowed IMC to receive more than 50 percent of its revenue from Medicare. (The waiver had been granted as part of an HMO pilot project that was set to expire. The renewal was ultimately not granted.)
But former Secretary Heckler herself, in a 2012 interview with HuffPost, confirmed that Jeb Bush did indeed lobby her personally — and that his input played a major role in her thinking. She was in favor of renewing the waiver, she said, although she left office before doing so.
She said she took his call, and took it seriously. “Jeb was one that I and friends of the Bushes always thought would be president,” Heckler said.
“He knew the people well,” said Heckler, referring to the South Florida Cuban community. “He was involved, and I know that his compassion and my sense of conscience and his, I thought, matched, and therefore I was positive, acting upon this.”
Heckler’s statement backs up congressional testimony offered by two other HHS officials in 1987. If all three are to be believed, Bush has been lying for some 20 years. He did, in fact, directly lobby the secretary for the IMC waiver.
The same year that the HHS officials testified, Recarey was indicted for defrauding Medicare, among other charges. He fled the country, first to Venezuela, then to Spain, where he fended off an extradition effort. It is alleged that he and IMC stole hundreds of millions of dollars overall. The IMC Medicare fraud is one of the largest in the program’s history.
‘A CLOSE PERSONAL RELATIONSHIP’
Heckler’s chief of staff, C. McClain Haddow, told a House Government Operations subcommittee in December 1987 that he was aware of Jeb Bush’s call to the secretary. “Ms. Heckler’s description of it and the reason why she thought it was important I thought were blatantly political,” he said. “She was just very interested in maintaining a close personal relationship with Mr. Bush, because she perceived there was a political future for her in doing so.” Heckler had been named ambassador to Ireland in 1985.
Jeb Bush’s version of events is different. As he told The Miami Herald in 1992, he could “recall making one phone call on behalf of IMC to an HHS official named Kevin Moley in the spring or summer of 1985. I asked that IMC be given a fair hearing, which IMC was given. No waiver was granted based on my phone call to Mr. Moley, and the accusation that millions of dollars were lost because of that call is unfair and untrue.”
Kristy Campbell, a spokeswoman for Bush, says that he does not recall phoning the cabinet secretary on behalf of Recarey. “As Governor Bush has said time and again, the only call he recollects making was to Mr. Moley. He was not a lobbyist and was not paid to make any calls,” she said.
But Moley, the person he acknowledges calling, who is himself a Bush ally, has said that Bush did in fact reach out to the secretary. Moley would be named assistant HHS secretary by President George H.W. Bush in 1989 and promoted to deputy secretary in 1992. He was an early donor to the presidential campaign of Jeb’s brother George W. Bush, and he gave $20,000 to the Republican National Committee in 2000 and another $25,000 in 2004, according to Federal Election Commission records. President George W. Bush named him permanent representative to the United Nations and other international organizations in Geneva in 2001.
Moley was an early supporter of Freedom’s Watch, a conservative advocacy organization launched late in George W. Bush’s tenure to defend the war effort and elect Republican politicians. (A co-founder of Freedom’s Watch, Sheldon Adelson, has since donated multimillions to GOP candidates, who court his favor.)
But like Haddow, Moley testified to Congress that Jeb Bush called the HHS secretary. “It came to my attention that Mr. Bush had contacted an official of the department” — his later testimony would make clear the official was Heckler — “to make an inquiry or to speak to the fact that Mr. Recarey was being hassled or whatever by federal officials on the 50-50,” explained Moley. “Jeb Bush is a person who I have known for some time. I called Jeb Bush when I heard this, and I said, ‘Jeb, this is something, you know, you probably don’t want to be involved in.’”
Bush made more than one call, according to testimony from Haddow. “Mr. Bush, in fact, called me at Ms. Heckler’s request at one point about this issue,” Haddow said.
SOUTH FLORIDA BUSINESS
Recarey’s problem was that health maintenance organizations like his were barred from receiving more than half of their revenue from Medicare reimbursement and his HMO’s waiver from the requirement was set to expire.
Moley told HuffPost in 2012 that Bush was just one of many power brokers who weighed in on Recarey’s case. “This guy bought up as much influence in the state of Florida as he could, Jeb being quite frankly the least of it,” Moley said, noting that a Republican senator and a Democratic congressman were among the many influential people to bend his ear for IMC.
Back in 1987, Moley testified that Bush had argued the 50 percent limit was arbitrary. “He said, ‘Kevin, I only want to make sure that Mike Recarey gets a fair hearing. He is down here in South Florida, and he, Mr. Recarey, indicates that he is being hassled on this arbitrary, bureaucratic 50-50 thing,’” Moley recalled. “I said, ‘Jeb, to be clear, that it is my office that is handling this.’ And Jeb chuckled, and that was the last conversation or any conversation that Mr. Bush, Mr. Jeb Bush, had in regard to IMC until we met socially some year or so later, and he casually brought up, ‘Gee, how is IMC doing?’ And I said, ‘Not so well,’ and he said that things had later come to his attention that indicated that he could understand that.”
“Not so well” was an understatement. A Medicare fraud investigator, Leon Weinstein, blew the whistle on Recarey in 1986, sparking congressional interest from then-Reps. Barney Frank (D-Mass.) and Pete Stark (D-Calif.). When Recarey fled, he left behind at least $230 million in unpaid medical claims, Pulitzer Prize-winning reporter Sydney Freedberg reported in The Wall Street Journal in a 1988 profile. He was taken into custody in Spain in 1993, but released a year later when the Spanish government rejected the U.S. extradition request, according to a December 1994 report by what is now the Government Accountability Office.
“Recarey stole a bunch of money from Medicare, and I spent a lot of time, along with the GAO, the FBI and other federal agencies trying to bring him to justice,” Stark told HuffPost in 2012. “It sure would have been nice if it all could have been prevented in the first place, but it’s clear he had friends in high places.”
The IMC allegations were not Recarey’s first brush with the law. His ties to Miami Cuban organized crime go back at least as far as the 1960s, Freedberg reported. He failed to file income tax returns in 1969 and 1970, even though he called himself an accountant. He spent a short time in prison for the tax evasion and, Freedberg reported, was ordered to be deported in 1964, an order that was clearly not successful.
So what was Jeb Bush paid tens of thousands of dollars to do for Recarey? “As it relates to my real estate work, my company received $75,000 in 1986 from IMC for extensive work that was documented and reported in a previous Miami Herald article but not mentioned in the April 26 story,” Bush told the Herald in 1992.
Bush’s Recarey connection flared up again briefly in 1995, when ABC’s “20/20” announced that it had interviewed the fugitive in Spain and that he had said the purpose of the payment was to buy influence, as reported at the time by the Sun Sentinel:
A fugitive accused of swindling millions from Medicare said he paid Jeb Bush $75,000 to buy influence in Washington while he tried to save his Florida health care company.
Miguel Recarey told ABC’s 20-20 that Bush’s father was vice president when the younger Bush called then-Health and Human Services Secretary Margaret Heckler on Recarey’s behalf.
A fugitive accused of swindling millions from Medicare said he paid Jeb Bush $75,000 to buy influence in Washington while he tried to save his Florida health care company.
Miguel Recarey told ABC’s 20-20 that Bush’s father was vice president when the younger Bush called then-Health and Human Services Secretary Margaret Heckler on Recarey’s behalf.
Asked whether he was paying for Bush’s influence, Recarey responded, “Sure. Obviously not enough.”
The Sun Sentinel story ran the day the “20/20” segment was scheduled to air, but something happened on the way to broadcast. Recarey, a fugitive at the time, saw the reports in the press and said that his comments had been taken out of context. ABC issued an apology to Bush and never ran the episode.
The network may have backed down too quickly. When he lobbied for Recarey, Jeb Bush wasn’t reaching out to just any Cabinet secretary: Heckler was a longtime family friend.
“My background with the Bushes is that I happen to be a big fan of Jeb Bush and of the Bush family,” Heckler told HuffPost. She said that when she was elected to Congress in 1966, she was the only woman among a freshmen class of 47. Rep. George H.W. Bush of Texas was elected class president.
“Since I was the only woman, he and I joined up for quite a few things,” she recalled. “The first press conference we had was on performing the ethical code of Congress for the House of Representatives. And that’s pretty much the way I look upon the whole Bush family and Bush himself.”
“George and Barbara,” Heckler said, are “two of the finest people ever to be in the White House.”
International Medical Centers HMO and Jeb Bush
https://en.wikipedia.org/wiki/Medicare_fraud
Medicare fraud
In the United States, Medicare fraud is the claiming of Medicare health care reimbursement to which the claimant is not entitled. There are many different types of Medicare fraud, all of which have the same goal: to collect money from the Medicare program illegitimately.[1]
The total amount of Medicare fraud is difficult to track, because not all fraud is detected and not all suspicious claims turn out to be fraudulent. According to the Office of Management and Budget, Medicare “improper payments” were $47.9 billion in 2010, but some of these payments later turned out to be valid.[2] The Congressional Budget Office estimates that total Medicare spending was $528 billion in 2010.[3]
Types
Medicare fraud is typically seen in the following ways:
- Phantom billing: The medical provider bills Medicare for unnecessary procedures, or procedures that are never performed; for unnecessary medical tests or tests never performed; for unnecessary equipment; or equipment that is billed as new but is, in fact, used.[4]
- Patient billing: A patient who is in on the scam provides his or her Medicare number in exchange for kickbacks. The provider bills Medicare for any reason and the patient is told to admit that he or she indeed received the medical treatment.
- Upcoding scheme and unbundling: Inflating bills by using a billing code that indicates the patient needs expensive procedures.[5][6]
- Kickbacks & Physician Self-Referrals: Kickbacks are bribes given in exchange for patient referrals to specific providers or facilities, or even a specific manufacturer of a drug or durable medical equipment. Similar to a kickback, a self-referral occurs when a physician refers a patient to a provider or entity with whom the physician has a financial relationship.[7]
A 2011 crackdown on fraud charged “111 defendants in nine cities, including doctors, nurses, health care company owners and executives” of fraud schemes involving “various medical treatments and services such as home health care, physical and occupational therapy, nerve conduction tests and durable medical equipment.”[8]
The Affordable Care Act of 2009 provides an additional $350 million to pursue physicians who are involved in both intentional/unintentional Medicare fraud through inappropriate billing. Strategies for prevention and apprehension include increased scrutiny of billing patterns, and the use of data analytics. The healthcare reform law also provides for stricter penalties; for instance, requiring physicians to return any overpayments to CMS within 60 days time.[9]
As of 2012, regulatory requirements tightened[10] and law enforcement has stepped up.[11][12][13]
However, in 2018, a CMS rule intended to limit upcoding was vacated by a judge;[14] it was later appealed in 2019.[15]
Law enforcement and prosecution

The Office of Inspector General for the U.S. Department of Health and Human Services, as mandated by Public Law 95-452 (as amended), is established to protect the integrity of Department of Health and Human Services (HHS) programs, to include Medicare and Medicaid programs, as well as the health and welfare of the beneficiaries of those programs. The Office of Investigations for the HHS, OIG collaboratively works with the Federal Bureau of Investigation in order to combat Medicare Fraud.[citation needed]
Defendants convicted of Medicare fraud face stiff penalties according to the Federal Sentencing Guidelines and disbarment from HHS programs. The sentence depends on the amount of the fraud. Defendants can expect to face substantial prison time, deportation (if not a US citizen), fines, and restitution[citation needed] or have their sentence commuted.[16]
In 1997, the federal government dedicated $100 million to federal law enforcement to combat Medicare fraud. That money pays over 400 FBI agents who investigate Medicare fraud claims. In 2007, the U.S. Department of Health and Human Services, Office of Inspector General, U.S. Attorney’s Office, and the U.S. Department of Justice created the Medicare Fraud Strike Force in Miami, Florida.[17] This group of anti-fraud agents has been duplicated in other cities where Medicare fraud is widespread. In Miami alone, over two dozen agents from various federal agencies investigate solely Medicare fraud. In May 2009, Attorney General Holder and HHS Secretary Sebelius Announce New Interagency Health Care Fraud Prevention and Enforcement Action Team (HEAT) to combat Medicare fraud.[18] FBI Director Robert Mueller stated that the FBI and HHS OIG has over 2,400 open health care fraud investigations.[19]
On January 28, 2010, the first “National Summit on Health Care Fraud” was held to bring together leaders from the public and private sectors to identify and discuss innovative ways to eliminate fraud, waste and abuse in the U.S. health care system.[20] The summit was part of the Obama Administration‘s effort to fight health care fraud.
From January 2009 to June 2012, the Justice Department used the False Claims Act to recover more than $7.7 billion in cases involving fraud against federal health care programs.[21]
Reporting by whistleblowers
The DOJ Medicare fraud enforcement efforts rely heavily on healthcare professionals coming forward with information about Medicare fraud. Federal law allows individuals reporting Medicare fraud to receive full protection from retaliation from their employer and collect up to 30% of the fines that the government collects as a result of the whistleblower’s information.[22] According to US Department of Justice figures, whistleblower activities contributed to over $13 billion in total civil settlements in over 3,660 cases stemming from Medicare fraud in the 20-year period from 1987 to 2007.[23]
International Medical Centers HMO and Jeb Bush
In 1985, Miguel G. Recarey Jr., CEO of International Medical Centers (IMC), a Florida-based health maintenance organization (HMO) was charged with bribing a Medicare officer, bribing a potential federal grand jury witness, and illegal wiretapping in U.S. District Court in Florida. He failed to appear for a hearing. Recarey received US$781 million in Medicare payments for 197 000 enrollees but did not pay doctors and hospitals for their care.[24] Recarey had “employed” Jeb Bush as a real estate consultant and paid him a US$75,000 fee for finding IMC a new location, although the move never took place. Bush lobbied the Reagan administration successfully on behalf of Recarey and IMC to waive a rule of maximum 50% Medicare enrollee proportion.[25][26] As of 2015, Recarey was a fugitive living in Spain.[26] The IMC fraud was then one of the largest in Medicare history.[27]
Columbia/HCA fraud case, 1996-2004
The Columbia/HCA fraud case is one of the largest examples of Medicare fraud in U.S. history. Numerous New York Times stories, beginning in 1996, began scrutinizing Columbia/HCA’s business and Medicare billing practices. These culminated in the company being raided by Federal agents searching for documents and eventually the ousting of the corporation’s CEO, Rick Scott, by the board of directors.[28] Among the crimes uncovered were doctors being offered financial incentives to bring in patients, falsifying diagnostic codes to increase reimbursements from Medicare and other government programs, and billing the government for unnecessary lab tests,[29] though Scott personally was never charged with any wrongdoing. HCA wound up pleading guilty to more than a dozen criminal and civil charges and paying fines totaling $1.7 billion. In 1999, Columbia/HCA changed its name back to HCA, Inc.
In 2001, Hospital Corporation of America (HCA) reached a plea agreement with the U.S. government that avoided criminal charges against the company and included $95 million in fines.[30] In late 2002, HCA agreed to pay the U.S. government $631 million, plus interest, and pay $17.5 million to state Medicaid agencies, in addition to $250 million paid up to that point to resolve outstanding Medicare expense claims.[31] In all, civil lawsuits cost HCA more than $1.7 billion to settle, including more than $500 million paid in 2003 to two whistleblowers.[30]
Omnicare fraud, 1999-2010
From 1999 to 2004, Omnicare a major supplier of drugs to nursing homes, solicited and received kickbacks from Johnson & Johnson for recommending that physicians prescribe Risperdal, a Johnson & Johnson antipsychotic drug to nursing home patients. During this time Omnicare increased its annual drug purchases from $100 million to more than $280 million.[32]
Starting in 2006, healthcare entrepreneur Adam B. Resnick sued Omnicare, under the False Claims Act, as well as the parties to the company’s illegal kickback schemes. Omnicare allegedly paid kickbacks to nursing home operators in order to secure business, which constitutes Medicare fraud and Medicaid fraud. Omnicare allegedly had paid $50 million to the owners of the Mariner Health Care Inc. and SavaSeniorCare Administrative Services LLC nursing home chains in exchange for the right to continue providing pharmacy services to the nursing homes.[33]
In November 2009, Omnicare paid $98 million to the federal government to settle five qui tam lawsuits brought under the False Claims Act and government charges that the company had paid or solicited a variety of kickbacks.[34] The company admitted no wrongdoing.[32]
In 2010, Omnicare settled Resnick’s False Claims Act suit that had been taken up by the U.S. Department of Justice by paying $19.8 million to the federal government, while Mariner and SavaSeniorCare settled for $14 million.[35][36]
Michigan Hematology-Oncology fraud
In 2013, Dr. Farid T. Fata was arrested on charges of providing chemotherapy treatments to patients who did not have cancer. Over a period of at least six years, Fata submitted US$34 million in fraudulent charges to private health practices and Medicare. At the time of his arrest, Fata owned Michigan Hematology-Oncology, one of Michigan’s largest cancer practices. In September 2014, Fata pled guilty to sixteen federal charges: thirteen counts of healthcare fraud, two counts of money laundering, and one count of conspiring to pay and receive kickbacks and cash payments for referring patients to a particular hospice and home health care company.[37] In addition to chemotherapy malpractice, the court found Fata guilty of mistreating patients with inappropriate octreotide, potent antiemetics, and parenteral vitamins.
Fata’s fraud scheme was discovered after one of his patients suffered an injury unrelated to his treatment. After beginning a lifelong chemotherapy treatment prescribed by Fata, patient Monica Flagg broke her leg and was seen by another physician at his practice, Dr. Soe Maunglay. Maunglay realized that Flagg did not have cancer and advised her to switch doctors immediately. Although he was already due to leave Fata’s practice over ethical concerns, Maunglay brought his concerns to the clinic’s business manager, George Karadsheh. Karadsheh filed a successful False Claims Act suit against Fata, leading to his arrest.[38] Barbara McQuade, the U.S. Attorney for the Eastern District of Michigan at the time, called the case “the most egregious case of fraud that [she had] ever seen in [her] life.”[39]
2010 Medicare Fraud Strike Task Force Charges
- In July 2010, the Medicare Fraud Strike Task Force announced its largest fraud discovery up until then, when charging 94 people nationwide for allegedly submitting a total of $251 million in fraudulent Medicare claims. The 94 people charged included doctors, medical assistants, and health care firm owners, and 36 of them have been found and arrested.[40][41] Charges were filed in Baton Rouge (31 defendants charged), Miami (24 charged) Brooklyn, (21 charged), Detroit (11 charged) and Houston (four charged).[40] By value, nearly half of the false claims were made in Miami-Dade County, Florida.[41] The Medicare claims covered HIV treatment, medical equipment, physical therapy and other unnecessary services or items, or those not provided.[42]
- In October 2010, network of Armenian gangsters and their associates used phantom healthcare clinics and other means to try to cheat Medicare out of $163 million, the largest fraud by one criminal enterprise in the program’s history up until then according to U.S. authorities[43] The operation was under the protection of an Armenian crime boss, known in the former Soviet Union as a “vor,” Armen Kazarian.[44] Of the 73 individuals indicted for this scheme, more than 50 people were arrested on October 13, 2010, in New York, California, New Mexico, Ohio and Georgia.[45][46]
2011 Medicare Fraud Strike Task Force Charges
In September 2011, a nationwide takedown by Medicare Fraud Strike Force operations in eight cities resulted in charges against 91 defendants for their alleged participation in Medicare fraud schemes involving approximately $295 million in false billing.[47]
2012 Medicare Fraud Strike Task Force Charges
In 2012, Medicare Fraud Strike Force operations in Detroit resulted in convictions[48] against 2 defendants for their participation in Medicare fraud schemes involving approximately $1.9 million in false billing.
Victor Jayasundera, a physical therapist, pleaded guilty on January 18, 2012, and was sentenced in the Eastern District of Michigan. In addition to his 30-month prison term, he was sentenced to three years of supervised release and was ordered to pay $855,484 in restitution, joint and several with his co-defendants.
Fatima Hassan, co-owned a company known as Jos Campau Physical Therapy with Javasundera, pleaded guilty on August 25, 2011, for her role in the Medicare fraud schemes and on May 17, 2012, was sentenced to 48 months in prison.
2013 Medicare Fraud Strike Task Force Charges
In May 2013, Federal officials charged 89 people including doctors, nurses, and other medical professionals in eight U.S. cities with Medicare fraud schemes that the government said totaled over $223 million in false billings.[49] The bust took more than 400 law enforcement officers including FBI agents in Miami, Detroit, Los Angeles, New York and other cities to make the arrests.[50]
2015 Medicare Fraud Strike Task Force Charges
In June 2015, Federal officials charged 243 people including 46 doctors, nurses, and other medical professionals with Medicare fraud schemes. The government said the fraudulent schemes netted approximately $712 million in false billings in what is the largest crackdown undertaken by the Medicare Fraud Strike Force. The defendants were charged in the Southern District of Florida, Eastern District of Michigan, Eastern District of New York, Southern District of Texas, Central District of California, Eastern District of Louisiana, Northern District of Texas, Northern District of Illinois and the Middle District of Florida.[51]
2019 Medicare Fraud Strike Task Force Charges
In April 2019, Federal officials charged Philip Esformes, 48 years old, of paying and receiving kickbacks and bribes in the then largest Medicare fraud case in U.S. history. The fraud took place between 2007 until 2016 and involved about $1.3 billion worth of fraudulent claims. Esformes was described as “a man driven by almost unbounded greed,”.[16] Esformes owned more than 20 assisted living facilities and skilled nursing homes.[52]
Former Hospital Executive Odette Barcha, 50, was Esformes’ accomplice along with Arnaldo Carmouze, 57, a physical assistant in the Palmetto Bay, Florida area. These three constructed a team of corrupt physicians, hospitals, and private practices in South Florida. The scheme worked as follows: bribes and kickbacks where paid to physicians, hospitals, and practices to refer patients to the facilities owned and controlled by Esformes. The assisted living and skilled nursing facilities would admit the patients and bill Medicare and Medicaid for unnecessary, fabricated and sometimes harmful procedures. Some of the charges to Medicare and Medicaid included prescription narcotics prescribed to patients addicted to opioids to entice the patients to stay at the facility in order for the bill to increase. Another technique was to move patients in and out of facilities when the patients had reached the maximum number of days allowed by Medicare and Medicaid. This was accomplished by using one of the corrupt physicians to see the patients and coordinate for readmission in the same or a different facility owned by Esformes. Per Medicare and Medicaid guidelines, a patient is allowed 100 days at a skilled nursing facility after a hospital stay. The patient is given an additional 100 days if the he/she spends 6 days outside of a facility or is readmitted to a hospital for 3 additional days. The facilities not only fabricated medical documents to show treatment was done to a patient, they also hiked up the prices to equipment and medications that were never consumed or used. Barcha as the Director of the Outreach program expanded the group of corrupt physicians and practices. She would advise the community physicians and hospitals to refer patients to the facilities owned by Esformes in exchange for monetary gifts. The law against kickbacks is called the Anti-Kickback Statute or Stark Law, which makes it illegal for medical providers to refer patients to a facility owned by the physician or a family member for services billable to Medicare and Medicaid. It also prohibits providers to receive bribes for patient referrals. Carmouze prescribed unnecessary prescription drugs to patients who may or may not have needed the medications. He also facilitated community physicians to visit the patient in the assisted living facilities owned by Esformes in order for the physician to bill Medicare and Medicaid, for which Esformes received kickbacks. Carmouze also assisted in falsifying medical documentation to represent proof of medical necessity for many of the medications, procedures, visits, and equipment charged to the government. Esformes has been detained since 2016. In 2019, he was convicted to 20 years in prison.[53]
On December 22, 2020, President Donald Trump commuted his sentence, upon suggestion by his son in law Jared Kushner and the Aleph Institute.[16]
See also
References
- “Medicare Fraud and Fraud in Other Government Healthcare Programs”. Retrieved 2017-12-05.
- politifact.com (2011-01-04). Retrieved on 2011-01-05.
- “The Budget and Economic Outlook: Fiscal Years 2010 to 2020” (PDF). Congressional Budget Office. 26 January 2010. Retrieved 30 October 2014.
- Steven Greenhouse (July 10, 2009). “Brooklyn Doctor Charged With Workers’ Compensation Fraud”. The New York Times. Retrieved July 28, 2022.
- “Upcoding Fraud » Constantine Cannon”. Retrieved December 5, 2017.
- “Risk Adjustment Fraud » Constantine Cannon”. Retrieved December 5, 2017.
- “Medicare Fraud Whistleblower – Report Medicare Fraud Online”. Brown, LLC. Retrieved 2024-06-10.
- “hhs.gov”. hhs.gov. May 7, 2011. Retrieved January 2, 2012.
- Westgate, Aubrey (May 2012), Medicare Fraud and Abuse and Your Practice, Physicians Practice
- “cms.gov” (PDF). Retrieved 2012-01-02.
- “oig.hhs.gov” (PDF). Retrieved 2012-01-02.
- Allen, Greg (2010-02-23). “m.npr.org”. m.npr.org. Retrieved 2012-01-02.
- “Medicare Fraud Reporting Center – Report Medicare Fraud Here – What is Medicare Fraud?”. Medicarefraudcenter.org. Retrieved 2012-01-02.
- “More Medicare Advantage upcoding could follow court ruling”. Modern Healthcare. 2018-09-12. Retrieved 2019-05-26.
- “CMS appeals ruling on Medicare Advantage overpayments: 4 things to know”. www.beckershospitalreview.com. Becker’s Hospital Review. 16 November 2018. Retrieved 2019-05-26.
- Vogel, Kenneth P.; Lipton, Eric; Drucker, Jesse (2020-12-24). “Behind Trump Clemency, a Case Study in Special Access”. The New York Times. ISSN 0362-4331. Retrieved 2023-09-26.
- Feds Fight Rampant Medicare Fraud in South Florida. NPR. Retrieved on 2010-11-04.
- Attorney General Holder and HHS Secretary Sebelius Announce New Interagency Health Care Fraud Prevention and Enforcement Action Team. Hhs.gov (2010-10-18). Retrieved on 2010-11-04.
- Johnson, Carrie (June 25, 2009). “53 in Detroit and Miami Indicted in Medicare Fraud Sting”. The Washington Post. Retrieved May 12, 2010.
- Health & Human Services Secretary Kathleen Sebelius, Attorney General Eric Holder Convene National Summit on Health Care Fraud, Unveil Historic Commitment to Fighting Fraud in President’s FY 2011 Budget. Hhs.gov (2010-10-18). Retrieved on 2010-11-04.
- “New Jersey Hospital Pays U.S. $8,999,999 to Settle False Claims Act Allegations”. US Department of Justice. 2012-06-21. Retrieved 2012-06-26.
- “Medicare Fraud Center – Report Medicare Fraud Here”.
- “Who can become a Medicare fraud whistleblower?”.
- “Alleged misconduct by international medical centers: statement of David C Williams, Director Office of Special Investigations” (PDF). GAO. 1987-12-15.
- Campbell, Duncan “The Bush dynasty and the Cuban criminals.” Archived August 26, 2013, at the Wayback Machine The Guardian (December 2, 2002). Retrieved October 8, 2023.
- Washington Post (2015-03-15). “Jeb Bush’s tie to fugitive Miguel Recarey goes against business-savvy image he promotes”. Tampa Bay Times. Retrieved 2023-09-26.
- Ryan Grim (2015-02-20). “When Dad Was VP, Jeb Bush Lobbied The Administration For A Medicare Fraudster”. Huffington Post. Retrieved 2023-09-26.
- Moewe, M.C. (April 17, 2006). “Jacksonville Business Journal Friday, April 14, 2006”. Jacksonville.bizjournals.com. Retrieved 2012-01-02.
- Bringing HCA Back to Life After years of scandal. Fortune Magazine Feb 2004
- M.C. Moewe (April 14, 2006). “Ex-Columbia chief helps grow Solantic”. Jacksonville Business Journal.
- Julie Appleby (December 18, 2002). “HCA to settle more allegations for $631M”. USA Today.
- Hilzenrath, David S. (January 16, 2010). “Justice suit accuses Johnson & Johnson of paying kickbacks”. The Washington Post. Retrieved January 17, 2010.
- U.S. Department of Justice (March 4, 2009). “Complaint of the United States in the District Court of Massachusetts CA No. 06-10149 RGS” (PDF).
- Department of Justice (November 3, 2009). “Nation’s largest nursing home pharmacy and drug manufacturer to pay $112 million to settle false claims act cases”.
- Ameet, Sachdev (February 11, 2010). “Scheme’s victims seeking restitution FDIC could get most of payment;”. Chicago Tribune. Archived from the original on October 29, 2013. Retrieved 12 September 2013.
- “Prominent New York City Real Estate Investor, Attorney and Atlanta Nursing Home Chains Pay $14 Million to Settle Whistleblower Kickback Case” (Press release). PR Newswire. Retrieved 12 September 2013.
- Steensma, David P. (January 2016). “The Farid Fata Medicare Fraud Case and Misplaced Incentives in Oncology Care”. Journal of Oncology Practice. 12 (1): 51–54. doi:10.1200/JOP.2015.008557. ISSN 1554-7477. PMID 26733620.
- Team, Legal (2022-04-11). “Can a Personal Injury Client Have a Whistleblower Case?”. YoumanCaputo. Retrieved 2023-03-07.
- Sweeney, Evan (January 18, 2016). “How a broken leg set off the fraud investigation against Farid Fata | Fierce Healthcare”. Fierce Healthcare. Retrieved March 7, 2023.
- Federal Bureau of Investigation press release, July 16, 2010, Medicare Fraud Strike Force Charges 94 Doctors, Health Care Company Owners, Executives, and Others for More Than $251 Million in Alleged False Billing
- Miami Herald, Feds charge 94 medicare suspects in Miami other cities, July 17, 2010, Jay Weaver
- Authorities charge 94 suspects for medicare fraud, PBS Newshour, July 16, 2010, accessed July 17, 2010, Lea Winerman
- Hairenik (14 October 2010). “Dozens of Armenians Charged with Largest Medicare Scam Ever”. armenianweekly.com.
- “Armenian gangsters charged in $160M Medicare scam”. nypost.com. 14 October 2010.
- Ailsa Chang (October 14, 2010). “52 arrested in sweeping Medicare fraud case”. National Public Radio. Retrieved October 18, 2010.
- “Feds take down largest-ever Medicare fraud ring”. Mass Device. October 14, 2010. Retrieved October 18, 2010.
- “Medicare Fraud Strike Force Charges 91 Dr Barbour of Palm Springs CaIndividuals for Approximately $295 Million in False Billing” (Press release). U.S. Department of Justice. September 7, 2011. Retrieved September 10, 2011.
- “Co-Owner of Detroit-Area Therapy Company Sentenced to 30 Months for Medicare Fraud Scheme”. U.S. Department of Justice. 2012-06-07. Retrieved 2012-06-14.
- Recent Medicare Fraud Scams and Busts Hank Pomeranz, Retrieved May 23, 2013.
- U.S. charges 89 people in Medicare fraud schemes U.S. Department of Justice: Retrieved May 14, 2013.
- National Medicare Fraud Takedown Results in Charges Against 243 Individuals for Approximately $712 Million in False Billing U.S. Department of Justice: Retrieved June 23, 2015.
- O’Keeffe, K (July 23, 2016). “Justice department charges three in $1 billion medicare fraud scheme in Florida; prosecutors outline details of its largest-ever single criminal health-care fraud case”. Wall Street Journal. ProQuest 1806148256.
- “Fla. healthcare executive found guilty in $1B Medicare fraud case”. Modern Healthcare. 2019-04-05. Retrieved 2019-07-31.
External links
- Stop Medicare Fraud site by US Government
- Fraud Overview at Medicare.gov site
- FBI.gov
Fund Raiser need a new computer mine was hit on internet. Plus internet server costs.
$500.00 May 2025.
Please Copy and Paste the below link into your browser to Help.
https://www.paypal.com/paypalme/SWebb822
Thank You for your support.
Contributions by Mail:
Stew Webb
913-944-5189
PO Box 13538
Overland Park, Kansas 66282
#news
#newsshorts
#shorts
#financialnews
#politics
#USAGPamBond
#USPresidentTrump
#USGrandJuryDemand
#StewWebbWhistleblower









.jpg)